April 29, 2020
On April 10, Centers for Medicare & Medicaid Services (CMS) issued the FY2021 SNF PPS Proposed Rule, which would take effect on October 1, 2021. The Proposed Rule includes updated payment rates used under the SNF PPS for fiscal year 2021 and changes to certain case-mix classification code mappings. Additionally, the rule includes a proposal to adopt the recent revisions to the statistical area delineations used for the SNF PPS, as well as proposals for the SNF Value-Based Purchasing (VBP) Program that affects Medicare payment to SNFs.
The highlights of the Proposed Rule include:
- An overall payment rate adjustment of 2.3%
- Adoption of the the Office of Management and Budget’s (OMB) most recent geographical delineations identifying a provider as either an urban or rural facility
- Changes to the Case-mix Classification Code Mappings
- Changes to the Skilled Nursing Facility Value-Based Purchasing Program (VBP)
- PDPM Discussion
Payment Rate Adjustment:
The Proposed Rule provides a 2.3 percent payment update for skilled nursing facilities for fiscal year 2021, representing an increase of $784 million compared to fiscal year 2020. CMS also confirms that SNFs that fail to submit data as required by the SNF Quality Reporting Program (QRP), will have the 2.0 percent reduction to the base rate applied.
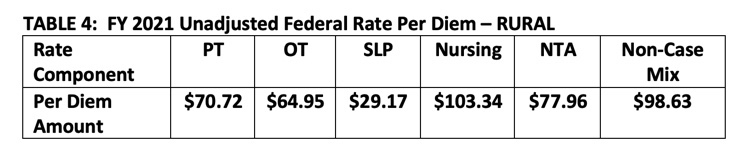
Tables 3 and 4 below are taken directly from the proposed rule and reflect the updated unadjusted federal rates for FY 2021, prior to adjustment for case-mix or Value-Based Purchasing.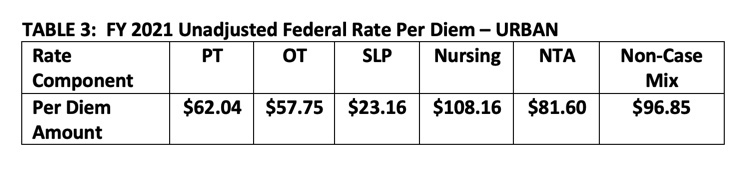
Revisions to Statistical Area Delineations (Urban and Rural)
The rule includes a proposal to adopt the most recent Office of Management and Budget (OMB) delineations used to identify a provider’s geographical status as either an urban or rural facility and to calculate the provider’s wage index. This delineation then has an impact on the facilities adjusted base rates, and revised OMB delineations shift some urban counties to rural and some rural counties to urban.
The Proposed Rule adopting the OMB delineations would modify a total of 47 counties that are currently located in rural areas to urban areas and shift 34 counties from urban core-based statistical areas (CBSAs) to rural areas. These new classifications would be used as the basis for determining the payment rates for these facilities beginning October 1, 2020 (see tables 3 and 4).
In the Proposed Rule, CMS does recognize that rural areas typically have lower area wage index values than urban areas, and SNFs located in these counties may experience a negative impact in their SNF PPS payment due to the proposed adoption of the revised OMB delineations. To mitigate the potential negative impacts the rule proposes applying a five percent cap on any decrease in a SNF’s wage index from the SNF’s wage index from the prior fiscal year. This transition would allow the effects of adopting the revised OMB delineations to be phased in over two years, where the estimated reduction in an SNF’s wage index would be capped at 5 percent in FY 2021. This transition policy would be for a one-year period, going into effect October 1, 2020, and continuing through September 30, 2021.
Case-mix Classification Code Mappings
The rule proposes changes to the code mappings used under the SNF PPS for classifying patients into case-mix groups. Under the PDPM, patients are classified into clinical categories based on the primary SNF diagnosis. The clinical classification may change based on whether the patient had a major procedure during the prior inpatient stay that impacts the plan of care as captured in items J2100 through J5000 on the MDS. In the current ICD-10 to clinical category mapping being used in FY 2020, ICD-10 codes associated with certain cancers that could require a major procedure do not include the option of a major procedure in the prior inpatient stay that may impact the plan of care. The rule proposes to add the surgical clinical category options of “May be Eligible for the Non-Orthopedic Surgery Category” or “May be Eligible for One of the Two Orthopedic Surgery Categories” to the clinical category mapping of the a number of cancer diagnoses when a major procedure, as described previously, is identified on the MDS.
The rule also outlines some proposed changes to clinical categories that certain codes currently map to:
- In the FY 2020 ICD-10 clinical category mappings, certain fracture codes map to the surgical default clinical categories such as “Orthopedic Surgery (Except Major Joint Replacement or Spinal Surgery)” or “Major Joint Replacement or Spinal Surgery” even if no surgery was performed. Given the concern raised by stakeholders, we propose to change the default clinical category for these codes to “Non-Surgical Orthopedic”, with the surgical option of “May be Eligible for One of the Two Orthopedic Surgery Categories.”
- The rule further proposes to change the default clinical category of a set of fracture codes to “Return to Provider” because these codes are unspecific and lack the level of detail provided by more specific codes as to whether the condition is on the right or left side of the body.
- A set of spinal stenosis codes currently have a default clinical category mapping of “non-surgical Orthopedic/Musculoskeletal” with no surgical option, which does not allow for coding in cases where patients have spinal stenosis and spinal laminectomy surgery. CMS proposes to add the surgical option of “May be Eligible for One of the Two Orthopedic Surgery Categories” to this set of codes.
Skilled Nursing Facility Value-Based Purchasing Program (VBP)
The SNF VBP scores SNFs on a single all-cause measure of hospital readmission. The Program aims to improve quality of care by incentivizing SNFs to reduce unplanned hospital readmissions.
CMS is proposing several minor changes including:
- Amending the definition of “SNF Readmission Measure” to “Skilled Nursing Facility Potentially Preventable Readmission after Hospital Discharge.” This is consistent with the name change that was finalized in the FY2020 SNF PPS Final Rule. This measure will eventually replace the currently used “Skilled Nursing Facility 30-day All-Cause Readmission Measure (SNFRM).”
- Indicating that VBP performance information will be publicly reported on the Nursing Home Compare Website or a successor website. “Successor website” language is included because CMS has plans to update the Nursing Home Compare website, including a name change.
- Establishing performance periods and performance standards for upcoming years.
CMS is also proposing to apply the 30-day Phase One Review and Correction deadline to the baseline period quality measure quarterly report, which is typically issued by CMS in December. According to CMS, this proposal would align the Phase One Review and Correction deadlines for the quarterly reports that contain the underlying claims and measure rate information for the baseline period or performance period. Under this proposal, SNFs would have 30 days following issuance of those reports to review the underlying claims and measure rate information. Should a SNF believe that any of the information is inaccurate, it may submit a correction request within 30 days following issuance of the reports.
PDPM Discussion
The proposed rule does not include any changes to any of the PDPM Classification categories nor the case-mix index weights assigned to any of the case-mix groups as finalized for FY2020.
The rule does state that “We would note that we continue to monitor the impact of PDPM implementation on patient outcomes and program outlays, though we believe it would be premature to release any information related to these issues based on the amount of data currently available. We hope to release information in the future that relates to these issues. We also continue to monitor the impact of PDPM implementation as it relates to our intention to ensure that PDPM is implemented in a budget neutral manner.”
The rule goes on to say “In future rulemaking, we may reconsider the adjustments made in the FY 2020 SNF PPS final rule to the case-mix weights used under PDPM to ensure budget neutrality and recalibrate these adjustments as appropriate, as we did after the implementation of RUG-IV in FY 2011. We invite comments from stakeholders on any observations or information related to the impact of PDPM implementation on providers or on patient care.”
CMS invites comments from stakeholders on any observations or information related to the impact of PDPM implementation on providers or on patient care. Comments will be accepted through June 9, 2020.




